We at OB/GYN Reform are demanding a Congressional investigation into the decades-long practice of removing healthy ovaries in women without proven increased risk of breast or ovarian cancer. We believe the government's failure to regulate a multi-billion dollar industry has left room for that industry's judgment to spiral out of control, resulting in serious health crises in women of an age, where health issues are not considered or addressed, who have become a profit center for this specialty. The 740,000 annual elective hysterectomies 242-244 in this country (those not to treat diagnosed cancer, source: AHRQ & CDC) cost an average of $33,130 per surgery according to the AHRQ. That's $24,516,200,000 a year.
Can 40% of a 160 million person population (source: HHS) truly require an elective major surgery? Why is no one asking this question?
Why does removal of healthy ovaries matter? Because, despite the fact that only 2% of all women are able to be diagnosed with a genetic predisposition to breast or ovarian cancer and might benefit from this surgery, the OB/GYN medical specialty removes the ovaries at time of hysterectomy for benign conditions like fibroids or endometriosis a staggering 55% of the time. (This percentage may be higher, but the CDC stopped publishing this data in 2000. We know it is very unlikely to be lower because it has risen from 25% in 1965 to 40% in 1984 to 55% in 1999.) It is also done in an additional 300,000 women who have benign ovarian cysts, which brings the number to at least 700,000 women a year.
In fact, this year, scientists finally began to ask how helpful this surgery has been in the reduction of BRCA 1/2 breast cancer. The answer? It has not been. (Read more here.)
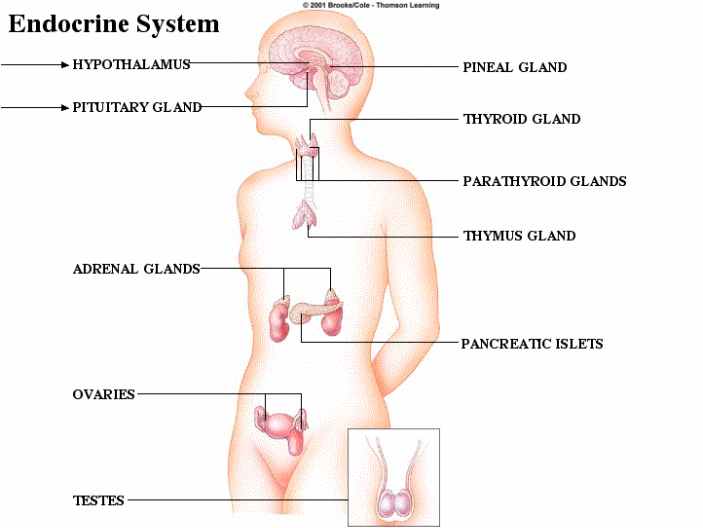
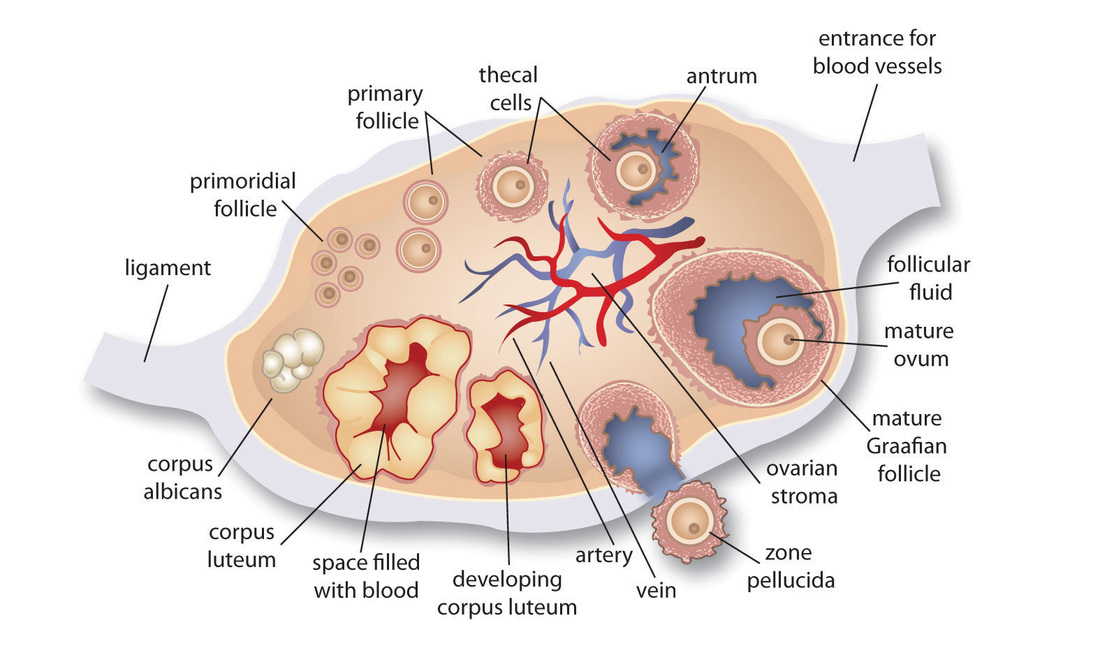
The ovaries are not, as commonly believed outside of medicine, part of a hysterectomy. Hysterectomy only includes the uterus, and possibly, cervix. The ovaries are part of both the exocrine (ducted, in this case, egg-producing) and the endocrine systems. It's proven that their endocrine function does not stop working at menopause, and many studies published in the American Congress of Obstetricians & Gynecologists' own medical journal detail the fact that this surgery leads to significantly increased risk of significantly premature mortality resulting from diseases including up to 7x risk of heart disease, 2x lung cancer, fracture due to severe osteoporosis, Alzheimer's and other forms of dementia, Parkinson's, and many more. Removing the ovaries does not result in "early menopause"; it results in sick women who die prematurely. The practice makes no sense and must stop immediately.
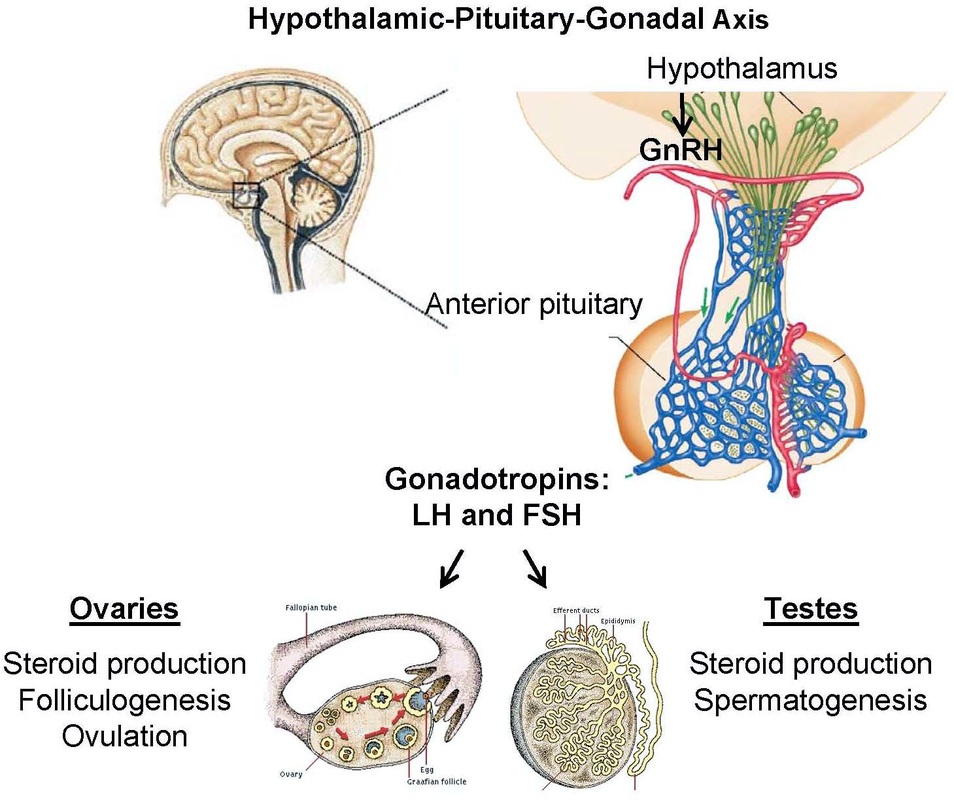
Under Section 1557 of the Affordable Care Act, women should be protected from disparate treatment in hospitals, the majority of which receive federal funding. Ovaries and testes are both gonads. They have homologous functions in the body's HPG axis. 1,000 healthy sets of ovaries are removed each day "to prevent cancer." Removing testes is the "gold standard" in preventing prostate cancer, which kills twice as many men each year as ovarian cancer kills women. How many preventative testis removals take place each day? Each year? It's never done. Though the mortality rate is double, the surgery is never performed in men without diagnosed cancer who've tried hormone suppressant treatment first.
We must thank Senator Mark Warner, who wrote on Aug. 6 to say, "Thank you for contacting me regarding issues with the professional judgment of OB/GYN doctors. I've taken the liberty of contacting the Food and Drug Administration on your behalf asking that they review your concerns and get back to me with a detailed and appropriate response. As soon as I receive a reply, I will again be in touch with you. To sign up for my newsletter please visit www.warner.senate.gov. Sincerely, MARK R. WARNER United States Senator"
However, we wrote to the FDA also, and they don't think they're the right agency since the issue is unrelated to pharmaceuticals and devices.
We must also thank Virginia Governor Terry McAuliffe for sending the issue to the Virginia health department for a response on August 28, and Congressman Gerry Connolly for writing to Dr. Nancy Lee, head of Women's Health within the Department of Health & Human Services on September 1, 2015.
These are important steps, but the most important is a Congressional hearing. Why? Because there is no possibility that any health advisory group can come back with the opinion that disassembling healthy endocrine systems is ever ok. Because there is no question that the removal of healthy ovaries, which is done a staggering 1,900 times a day, is harmful. The OBGYN specialty has things to answer for. We need access to a forum to share the harm these surgeries have done to millions of women, and to put an end to these types of surgery once and for all.
www.gynreform.com
Can 40% of a 160 million person population (source: HHS) truly require an elective major surgery? Why is no one asking this question?
Why does removal of healthy ovaries matter? Because, despite the fact that only 2% of all women are able to be diagnosed with a genetic predisposition to breast or ovarian cancer and might benefit from this surgery, the OB/GYN medical specialty removes the ovaries at time of hysterectomy for benign conditions like fibroids or endometriosis a staggering 55% of the time. (This percentage may be higher, but the CDC stopped publishing this data in 2000. We know it is very unlikely to be lower because it has risen from 25% in 1965 to 40% in 1984 to 55% in 1999.) It is also done in an additional 300,000 women who have benign ovarian cysts, which brings the number to at least 700,000 women a year.
In fact, this year, scientists finally began to ask how helpful this surgery has been in the reduction of BRCA 1/2 breast cancer. The answer? It has not been. (Read more here.)
The ovaries are not, as commonly believed outside of medicine, part of a hysterectomy. Hysterectomy only includes the uterus, and possibly, cervix. The ovaries are part of both the exocrine (ducted, in this case, egg-producing) and the endocrine systems. It's proven that their endocrine function does not stop working at menopause, and many studies published in the American Congress of Obstetricians & Gynecologists' own medical journal detail the fact that this surgery leads to significantly increased risk of significantly premature mortality resulting from diseases including up to 7x risk of heart disease, 2x lung cancer, fracture due to severe osteoporosis, Alzheimer's and other forms of dementia, Parkinson's, and many more. Removing the ovaries does not result in "early menopause"; it results in sick women who die prematurely. The practice makes no sense and must stop immediately.
Under Section 1557 of the Affordable Care Act, women should be protected from disparate treatment in hospitals, the majority of which receive federal funding. Ovaries and testes are both gonads. They have homologous functions in the body's HPG axis. 1,000 healthy sets of ovaries are removed each day "to prevent cancer." Removing testes is the "gold standard" in preventing prostate cancer, which kills twice as many men each year as ovarian cancer kills women. How many preventative testis removals take place each day? Each year? It's never done. Though the mortality rate is double, the surgery is never performed in men without diagnosed cancer who've tried hormone suppressant treatment first.
We must thank Senator Mark Warner, who wrote on Aug. 6 to say, "Thank you for contacting me regarding issues with the professional judgment of OB/GYN doctors. I've taken the liberty of contacting the Food and Drug Administration on your behalf asking that they review your concerns and get back to me with a detailed and appropriate response. As soon as I receive a reply, I will again be in touch with you. To sign up for my newsletter please visit www.warner.senate.gov. Sincerely, MARK R. WARNER United States Senator"
However, we wrote to the FDA also, and they don't think they're the right agency since the issue is unrelated to pharmaceuticals and devices.
We must also thank Virginia Governor Terry McAuliffe for sending the issue to the Virginia health department for a response on August 28, and Congressman Gerry Connolly for writing to Dr. Nancy Lee, head of Women's Health within the Department of Health & Human Services on September 1, 2015.
These are important steps, but the most important is a Congressional hearing. Why? Because there is no possibility that any health advisory group can come back with the opinion that disassembling healthy endocrine systems is ever ok. Because there is no question that the removal of healthy ovaries, which is done a staggering 1,900 times a day, is harmful. The OBGYN specialty has things to answer for. We need access to a forum to share the harm these surgeries have done to millions of women, and to put an end to these types of surgery once and for all.
www.gynreform.com






 RSS Feed
RSS Feed
